TMJ, or Temporomandibular Joint Disorder, is a problem that can feel confusing. If you experience the symptoms of this condition, you may not know where to turn. Do you see your medical doctor for pain in the jaw, head, or neck, or do you see your dentist? The team at the Cosmetic Dentists of Austin in Austin, TX have a unique educational background that enables our dentists to accurately diagnose TMJ disorder and treat the underlying problem so function and comfort can be restored.
What Is TMJ / TMD?
TMJ and TMD are acronyms commonly used to describe a condition affecting the temporomandibular joints, which are critical components of the jaw structure. The TMJ, or temporomandibular joint, is located on each side of the jaw, just in front of the ears, and connects the lower jaw (mandible) to the skull (temporal bone). These joints are among the most complex in the body, allowing for a wide range of movement, including opening, closing, sliding, and grinding of the jaw.
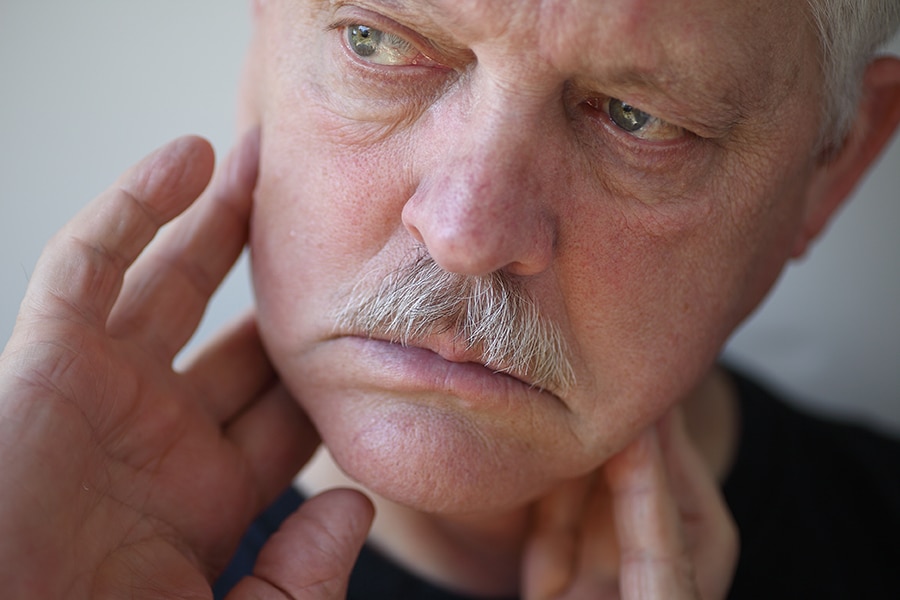
TMD, or Temporomandibular Joint Disorder, encompasses a group of symptoms that arise when these joints and the associated muscles and ligaments fail to function properly. This dysfunction can lead to inflammation and pain in the TMJ, manifesting in a variety of symptoms that can affect eating, speaking, and even the comfort of facial expressions.
The causes of TMD are diverse and can include direct injury to the joint, arthritis, excessive strain from habits like teeth grinding (bruxism) or clenching, poor dental alignment (malocclusion), or stress-induced muscle tension. These factors can lead to a compromised TMJ, where the joint becomes inflamed, and the normal movement is disrupted.
Inflammation of the TMJ can result from various issues, such as mechanical wear and tear, misalignment of the teeth or jaw, or overuse from repetitive actions like chewing gum excessively. This inflammation can cause symptoms ranging from mild discomfort to severe pain, and it can affect not only the joint itself but also the surrounding muscles and ligaments. Symptoms may include jaw pain, difficulty in opening or closing the mouth, a clicking or grinding noise during jaw movement, earaches, headaches, and even neck and shoulder pain.
Understanding TMJ and TMD is essential for identifying the appropriate treatment options. Proper diagnosis involves examining the physical function of the jaw and surrounding muscles, as well as understanding the patient’s dental history and lifestyle factors that may contribute to the condition. By addressing the root causes of TMD, rather than just the symptoms, a more effective and long-term solution can be achieved, improving the patient’s quality of life and overall oral health.
What Are The Symptoms Of TMJ / TMD?
The most common symptom of Temporomandibular Joint Disorder (TMJ/TMD) is popping or clicking sounds when you open and close your mouth, which may or may not be accompanied by pain. However, the range of symptoms is broad and can vary significantly in severity, encompassing general tension in the jaw or face, ringing in the ears (tinnitus), dizziness, neck pain, and chronic headaches, including migraines. Some patients may also experience earaches, difficulty chewing or a sudden uncomfortable bite, as if the upper and lower teeth are not fitting together properly.
In severe cases, locking of the jaw can occur, making it difficult to open or close the mouth completely. Symptoms can extend beyond the jaw and neck, leading to back pain and even affecting posture. The complexity and variability of these symptoms often present a challenge in reaching an accurate diagnosis. Our team at The Cosmetic Dentists of Austin uses specific instruments and protocols to meticulously observe the structure of the jaw and its functionality, allowing us to identify the triggers for these uncomfortable symptoms and tailor a treatment plan suited to each individual’s condition.
What Causes TMJ / TMD?

Research suggests various potential causes of Temporomandibular Joint Disorder (TMD), and it is often the interplay of several factors that leads to the development of this condition, which is still not fully understood. One common cause is excessive gum chewing, which can place undue strain on the joint and its supporting muscles. Bruxism, or teeth grinding, is another significant factor, often exacerbated by stress and anxiety. These psychological factors can lead to unconscious jaw clenching and grinding, particularly during sleep, further stressing the TMJ.
Trauma to the jaw, such as a heavy blow or whiplash injury, can directly damage the joint or disrupt its normal functioning. Malocclusion, or a bad bite, where the upper and lower teeth do not align properly, can also contribute to TMD by causing an uneven distribution of force during chewing and speaking.
Poor posture, especially in the neck and upper back, can lead to muscle strain and alignment issues, affecting the jaw’s position and function. Additionally, existing musculoskeletal disorders or conditions like arthritis can directly affect the temporomandibular joints, leading to degeneration or inflammation of the joint.
Other contributing factors can include hormonal changes, particularly in women, who are more prone to developing TMD. Certain habits, like biting nails or chewing on pencils, can also put extra stress on the jaw joints and muscles. Genetic predispositions may play a role in the susceptibility to TMD, with some individuals having a natural predisposition to pain sensitivity and joint problems. Understanding these multifaceted and interconnected causes is crucial for diagnosing and effectively treating TMD.
Can I Treat TMJ / TMD On My Own?
Some instances of Temporomandibular Joint Disorder (TMD), particularly those related to excessive stress on the jaw like bruxism, may be managed with self-care practices. Minor and temporary symptoms can often be alleviated through lifestyle modifications, such as:
- Applying ice or cold packs to the cheek for a few minutes: This can help reduce inflammation and numb the area, providing temporary relief from pain.
- Taking over-the-counter anti-inflammatory medication: Medications such as ibuprofen can reduce swelling and alleviate pain, but they should be used as directed to avoid long-term side effects.
- Developing stress management strategies: Activities like yoga, meditation, or even regular exercise can help reduce overall stress levels, potentially decreasing the frequency and severity of jaw clenching and grinding.
- Eating soft foods: Opt for foods that require less chewing, such as soups, stews, smoothies, and cooked vegetables, to give your jaw a rest.
- Avoiding habits that strain the jaw: Chewing gum, biting nails, or eating hard candies can exacerbate symptoms, so it’s best to avoid these activities until symptoms improve.
- Gentle massage and stretching exercises for the jaw and neck: This can help relieve muscle tension and improve range of motion. It’s important to perform these exercises gently and avoid overextending the jaw.
In addition to these measures, maintaining good posture, especially while working at a computer or looking at a phone, can help prevent neck and jaw strain. Using ergonomic pillows and practicing good sleep hygiene can also support proper alignment and reduce nighttime jaw clenching.
While these self-care strategies can be effective for temporary relief, they are not a substitute for professional care. If symptoms persist or worsen, or if you experience significant pain or dysfunction, it is crucial to seek evaluation and treatment from a dental professional experienced in treating TMD. Persistent or severe symptoms may indicate a more complex issue that requires comprehensive treatment to prevent long-term damage and alleviate chronic pain.
How Is TMJ / TMD Diagnosed?
The diagnostic process for TMD must go beyond the basic dental or physical examination. It is, therefore, best conducted by a dentist who has completed training in the area of neuromuscular dentistry. Dr. Schiro, Dr. Hay, and Dr. Barras attended courses at the esteemed Las Vegas Institute for Advanced Dental Studies. Their extensive training accommodates accurate diagnosis of muscular and joint conditions.

Step One: Consultation
Initial consultation for TMD diagnosis involves an in-depth conversation with your dentist. This dialogue provides us with valuable information that helps us tie symptoms into a potential cause. Questions that may be asked during your consultation include:
- Have you sustained an injury to the jaw or face?
- Where does pain occur and what is the intensity of pain?
- When does pain occur (triggers)?
- Do symptoms affect one or both sides of the face?
Step Two: Examination
A neuromuscular dental examination is performed to help us understand the physical state of the jaw and the temporomandibular joints. We may listen as you open and close your mouth and may gently palpate the joints as you do this.
The range of motion of your jaw will be observed, and the muscles around the TMJs will be felt.
Step Three: Diagnostic Tests
Physical examination alone is not sufficient to fully understand the nature of TMD in each case. We rely on data gathered by diagnostic imaging such as x-rays and, if necessary, ultrasound or other imaging types. Tests that we perform in our office include:
- BioPak, Electromyography, or EMG, monitors the electrical impulses of the muscles in the jaw. This test helps us recognize if jaw pain is stemming from the muscles themselves or from a structural irregularity.
- TENS therapy is used diagnostically to observe the jaw’s natural resting position.
How Is TMJ / TMD Treated In Austin?
TMD Treatment May Include:
- Continued treatment with TENS therapy to facilitate muscle relaxation in the jaw.
- Temporary use of an oral appliance, similar to a mouthguard, to support the retraining of jaw muscles.
- Structural changes in the form of porcelain crowns to support a balanced bite.
Neuromuscular dentistry is a valuable resource for patients with TMD. Give us a call to learn more about our diagnostic and treatment protocols.
Call us today at 512.333.7777 for your complimentary consultation, dental appointment, or if you just want more information about our Smile Makeovers in Austin Texas.
Frequently Asked Questions
How Long Does TMJ/TMD Treatment Typically Take?
The duration of treatment depends on the condition’s severity, underlying causes, and the chosen treatment plan. While some patients experience relief within a few weeks, more complex or severe cases may require several months of consistent care to fully resolve and restore proper jaw function.
Can TMJ/TMD Go Away On Its Own?
In some mild cases, TMJ symptoms may improve with rest, self-care practices, and avoiding jaw strain. However, persistent or worsening symptoms often require professional evaluation to prevent long-term damage, chronic discomfort, and ensure effective treatment.
Will I Need Surgery For My TMJ/TMD?
Surgery is rarely necessary for TMJ/TMD treatment. Non-invasive treatments, such as oral appliances, TENS therapy, or dental corrections, are often effective in managing most TMJ cases. Surgery is typically reserved for severe, unresponsive cases.
Can TMJ/TMD Cause Sleep Problems?
Yes, TMJ/TMD can contribute to disrupted sleep patterns, particularly if it causes nighttime teeth grinding (bruxism) or jaw clenching. These habits can lead to muscle tension, discomfort, and difficulty achieving restful sleep. Addressing TMJ dysfunction often improves overall sleep quality.
Can Lifestyle Changes Help with TMJ Treatment?
In addition to professional care, lifestyle adjustments such as stress management, improved posture, avoiding hard or chewy foods, using relaxation techniques, and incorporating gentle jaw exercises can help reduce symptoms and effectively support your treatment plan.
Why Choose The Cosmetic Dentists of Austin for TMJ Treatment?
When it comes to TMJ/TMD treatment, expertise, and advanced training are essential for effective, lasting results.
The Cosmetic Dentists of Austin team combines years of experience with specialized education to deliver exceptional care. Dr. John Christian Schiro, DDS, FAGD, is a graduate of the prestigious Las Vegas Institute for Advanced Dental Studies (LVI) and holds the elite Fellowship in the Academy of General Dentistry, a distinction earned by fewer than 1% of dentists nationwide. Dr. John D. Barras, DDS, LVIF, brings a passion for advanced neuromuscular dentistry, perfected through LVI’s rigorous training and years of experience caring for diverse patient needs, including underserved communities. Dr. John M. Hay, DDS, LVIF, has been serving Austin since 2008, dedicating his practice to transforming both oral health and overall well-being through the art and science of neuromuscular and cosmetic dentistry.
Together, their combined expertise and commitment to patient-centered care make The Cosmetic Dentists of Austin the trusted choice for restoring comfort, function, and quality of life.
Find Lasting TMJ Relief in Austin, TX
If you’re struggling with the discomfort and pain caused by TMJ/TMD, don’t wait to find the relief you deserve. At The Cosmetic Dentists of Austin, our team has the experience, training, and advanced technology to diagnose and treat TMJ disorders accurately. Treating the underlying cause allows us to relieve discomfort, restore normal jaw function, and help you feel your best.
Take the first step toward lasting relief—call us today at 512.333.7777 to schedule your consultation. We’re dedicated to helping you achieve a comfortable, confident smile you love!
